Match to COPD Clinical Trials
Chronic obstructive lung disease (COPD) is a lung condition that makes breathing, one of the most basic bodily functions, difficult. This disease can make everyday living harder, but not impossible. Currently, there are a variety of therapies, programs, and medicines available to patients to help alleviate COPD symptoms. Clinical research and trials that patients can easily participate in are also striving to discover new and improved ways to treat COPD. This guide is intended to help educate those living with COPD about the condition itself and about the resources available to help treat it.
About COPD
Chronic obstructive lung disease (COPD) is a lung condition that makes breathing difficult and that is currently incurable. There are two types of COPD, one caused by chronic bronchitis and the other caused by emphysema.
- Chronic Bronchitis
A condition where the bronchial tubes of the lungs become inflamed and produce extra mucus which impedes one’s airflow. - Emphysema
A disease where the lung’s air sacs become inflamed and ultimately damaged, making breathing difficult.
COPD can cause many symptoms which may interfere with the patient’s everyday life. The most common symptoms reported include, but are not limited to:
- Dyspnea, or breathlessness
- Wheezing
- Coughing
- Sputum, or mucus, production
The severity of patients’ symptoms may vary. Some may not even notice their symptoms, unless doing strenuous physical activities, while others may become out of breath from just dressing and undressing. It should be noted that these symptoms may be caused by another condition or disease, such as asthma, a respiratory infection, or lung cancer. One must contact his or her health care provider to receive a proper diagnosis.
Some diseases also naturally accompany COPD. These illnesses include, but are not limited to:
- Cardiovascular disease
- Metabolic syndrome
- Depression
- Lung cancer
- Skeletal muscle dysfunction
- Osteoporosis
- Anxiety
It is important for health care providers to actively search for and attend to these accompanying illnesses so that symptoms do not become worse.
COPD patients commonly experience flare ups, which are also known as exacerbations.
- Flare Ups
Periods of time where symptoms of a certain disease become worse in a patient.
Flare-ups are usually brought about when the patient has a cold, a flu, or an infection. They can be very dangerous because they could damage the lungs further. It is important to talk to a health care provider so that steps to prevent flare ups from happening can be taken.
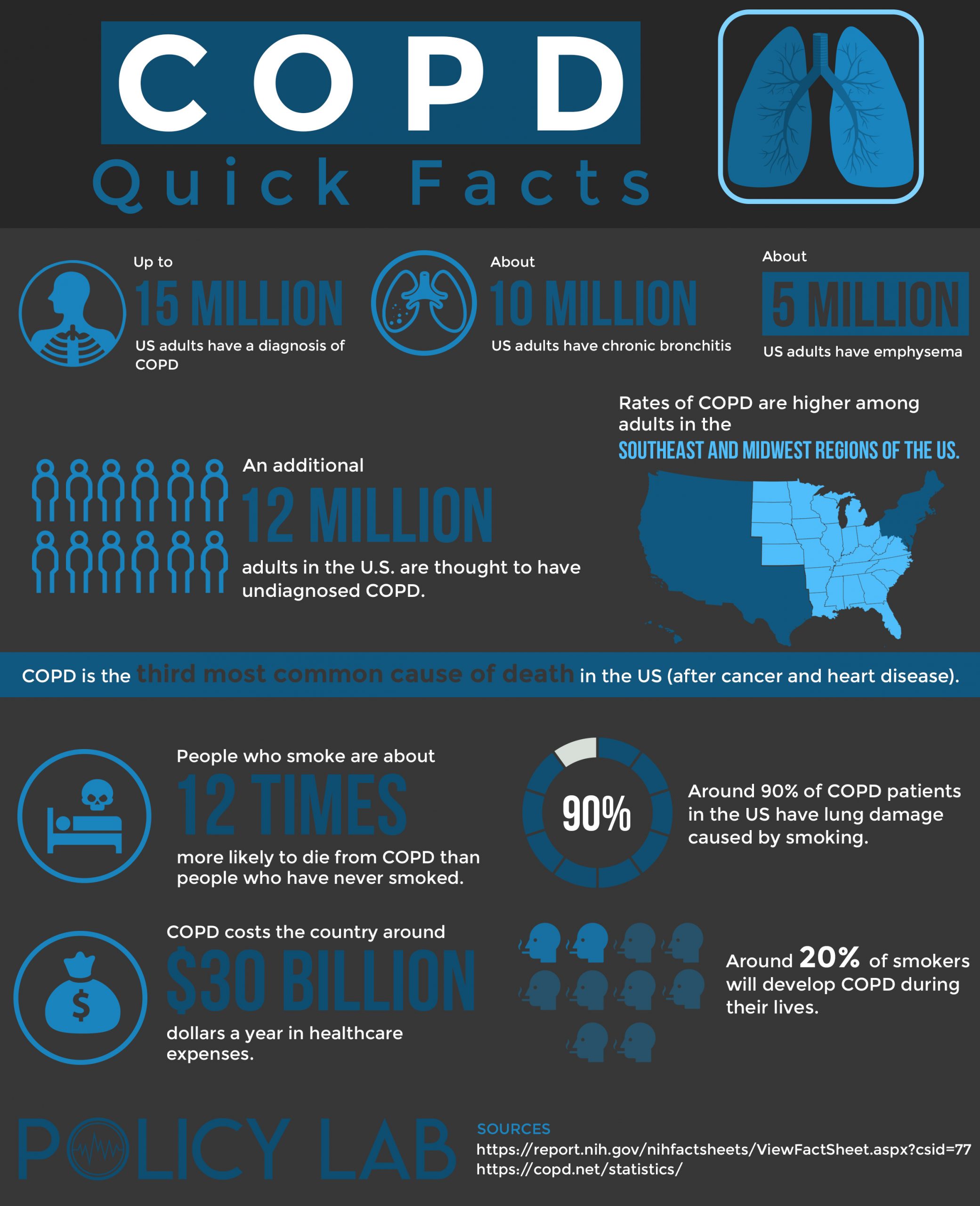
COPD Stastics
Causes Of COPD
COPD is usually caused by something noxious that irritates the lungs over an extended period of time. Although, there are other factors that may cause or increase the chances of acquiring this disease. These irritants and factors are discussed below.
Cigarette Smoking
The most efficient test on a person’s airflow which will recognize any breathing impediment. Results of a post-bronchodilator FEV1/FEV<0.70 would mean there is a breathing impediment. This test could recognize other conditions, like asthma, so it is important to combine the test results with the patient’s symptoms for proper diagnosis.
Pollution
Pollution is also a major irritant that can also cause COPD. This includes both indoor and outdoor pollutants. With the use of fossil fuels on the rise, more and more areas of the world are experiencing higher amounts of pollution in the air. Living in an area with high pollution rates may increase the risk of COPD. One of the most polluted areas in the United States is Los Angeles. Indoor pollution such as smoke from smoking indoors, aerosol sprays, and fumes from unclean furnaces or poorly ventilated cooking areas also can irritate the lungs.
Genetics
Genetics may put people at a higher risk of COPD. Some of these genetic factors include:
- Severe hereditary deficiency of alpha-1 antitrypsin (AATD)
- Lung development during childhood, like recurrent respiratory infections or low birth weight
- Female gender
Diagnosis
If a patient thinks he or she is think experiencing symptoms of COPD, it is advised to a healthcare provider as soon as possible for proper diagnosis. It is common for healthcare providers to take a detailed medical history and give a full physical exam. Other tests are also required. These tests include:
Spirometry
The most efficient test on a person’s airflow which will recognize any breathing impediment. Results of a post-bronchodilator FEV1/FEV<0.70 would mean there is a breathing impediment. This test could recognize other conditions, like asthma, so it is important to combine the test results with the patient’s symptoms for proper diagnosis.
Oxygen in the Blood
The normal amount of oxygen in the blood should be between 75 and 100 mm Hg. Anything under 75 would indicate a problem with the lungs, like COPD.
Chest X-Ray or Cat Scan
These will allow the doctor to view any abnormalities of the lungs.
COPD Assessment Test (Cat)
This test is a list of questions that can also help a physician diagnose a patient with COPD. The assessment test consists of symptoms the patient may be experiencing and a number scale to rank the severity of these symptoms. For example, “I never cough” compared to “I cough all the time.”
Match to COPD Clinical Trials
Treatment
Many medicines, methods, and programs are readily available to people living with COPD to help reduce their symptoms. Clinical research and trials are also helping to improve these treatments. The treatments are all listed below.
Medicine
Medicine is prescribed by a health care provider. Sometimes patients will be prescribed a combination of medicines to assess their individual needs. There are long acting and fast acting versions of these drugs.
- Long acting medicine – These medications are taken on a regular basis and help to continually reduce symptoms.
- Fast acting medicine – These medications are taken on a special occasion, usually when symptoms worsen and there is a flare up, to quickly reduce symptoms back to a normal level.
The medicines are either inhaled or ingested by pill. Common medications are listed as follows:
- Bronchodilators
- Beta-agonists (inhaled)
- Anticholinergics (inhaled)
- Phosphodiesterase-4 inhibitors (pill)
- Theophylline (pill)
- Steroids (inhaled or pill)
The medications that are inhaled can be taken by the following:
- Metered dose inhalers – This device distributes a specific amount of medication by spraying vaporized medication when one inhales. It is the most common way of taking medication for COPD patients.
- Dry powder inhalers – This device works the same as a metered dose inhaler but the medication is delivered through dry powder.
- Nebulizers – This device delivers the medication via mist and requires a face mask so that it may be breathed into the lungs for a certain amount of time.
Oxygen Therapy
Supplemental oxygen may be necessary if the blood is not receiving enough oxygen. The amount of oxygen needed varies from patient to patient, depending on the severity of their COPD. Oxygen treatment can have many benefits such as:
- Sleep improvement
- Mental function improvement
- Exercise improvement
Oxygen can be administered through several devices which include the following:
- Oxygen tanks
- Liquid oxygen systems
- Concentrators
These devices all deliver oxygen to the patient and are now available in portable forms so that users can live their everyday lives with no hassle.
Lifestyle Changes
Lifestyle changes can play a major role in alleviating the symptoms of COPD and in the overall health for patients. It is essential for patients to quit smoking and to exercise as these changes will have a major impact on their wellness. Both of these changes can be very difficult to achieve, so there are tips provided below to assist those with COPD.
How to quit smoking:
- Talk to a healthcare provider that can give medical advice on how and why to quit smoking.
- Try nicotine replacement therapy like nicotine gum and patches that will reduce the urge.
- Try prescription pills that can stop cravings and reduce withdrawals.
- Get support from loved ones and support groups.
- Exercise!
How to start exercising:
- Talk to a healthcare provider that can give medical advice on how and why to start exercising.
- Set goals.
- Exercise with groups of people or friends to help with motivation and accountability.
- Try a pulmonary rehabilitation program.
- Maintain a schedule.
Positive Attitude
A positive attitude can go a long way in the health of those with COPD. It is easy to feel extremely weighed down by COPD. Some common comorbidities that accompany this disease are depression and anxiety. A healthy mind is just as important as a healthy body. It is important to keep family members and friends close to help support those with COPD. It is also recommended to speak to a counselor who can guide those finding it hard to stay positive.
It is important for patients to remember that they are not alone, that they have many resources, and that they are not defined by this disease! Depression or anxiety must be assessed and proper treatment should be administered to avoid flare ups. For patients who think they may be suffering from anxiety or depression, they should speak to a health care provider as soon as possible.
Interview with an Expert

Dr. Lijo John
Dr. Lijo John is a community pharmacist with 9 years of experience and graduated from Rutgers University in 2012. He has extensive experience serving patients with a focus in geriatric medicine, diabetes management, and preventative medicine such as immunizations and lifestyle modification counselling. Dr. John also enjoys writing and presenting on complex medical topics aimed at the general population to drive positive behavioral change in topics such as vaccine hesitancy and smoking cessation.
An Overview of COPD
Chronic obstructive pulmonary disease (COPD) is a progressive and irreversible disease that is primarily caused by cigarette smoking as well as exposure to other toxins. It is the fourth leading cause of death in the United States. The only way to slow the progression of COPD is to stop smoking and avoid other toxins known to worsen the condition. 1
How Has Treatment Developed Over Time?
The current non-pharmacologic treatment paradigm includes inhaled pulmonary rehabilitation, which is exercise training to reduce symptoms of dyspnea and fatigue. If a patient’s COPD has progressed to the point of having reduced oxygen levels in the blood even at rest, they may benefit from supplemental oxygen therapy. This has been shown to reduce mortality. COPD patients are strongly advised to stay up to date with recommended vaccines as this can reduce the likelihood of respiratory infections that can lead to COPD exacerbations. Recommended vaccinations include the annual influenza vaccine, as well as the two pneumonia vaccines, PPSV23 and PCV13. 2
What is the Current Standard of Care?
Pharmacologic options for COPD are used to alleviate symptoms and do not improve survival rates like smoking cessation and oxygen therapy do. Short-acting bronchodilators are used as initial therapy and fall under two categories, short-acting beta agonists (SABA) and short-acting anti-muscarinic agents. They can be used for patients with occasional symptoms in addition to being used as rescue inhalers. Patients with more persistent symptoms can be treated with long-acting bronchodilators which include long-acting beta agonists (LABA) and/or long-acting muscarinic agents (LAMA). These agents provide significant improvement in symptoms, lung function as well as decreasing exacerbations, at the cost of increasing adverse effects. In patients with acute exacerbations of COPD, treatment includes increasing dose of bronchodilators and a course of systemic corticosteroids. Antibiotics are recommended in an acute exacerbation episode if the patient exhibits severe symptoms.2
What Are Some Newer Treatments?
In patients whose symptoms are not controlled with a single long-acting bronchodilator, a combination of LABA and LAMA is recommended. In recent years, several combination inhalers have been approved by the FDA to improve patient adherence and convenience, such as Anoro Ellipta3 (umeclidinium and vilanterol) and Stiolto Respimat4 (tiotropium and olodaterol). In those patients whose symptoms still persist and require an inhaled corticosteroid, Trelegy combines the LABA and LAMA with an inhaled corticosteroid (umeclidinium, vilanterol, and fluticasone furoate)5. Daliresp (roflumilast) is a newer option for patients who are already on inhalers and suffer 2 flare-ups within the last 12 months6. This oral medication can reduce inflammation in the lungs and airways. In advanced emphysema, endobranchial valve (EBV) implantation can also provide improvement in symptoms and lung function6. The long term role of this device is still being studied.
What New Clinical Trials Are Currently Being Ran?
There are new molecules being studied for this disease including new combination inhalers7, dual inhaler with a new mechanism of action (Ensifentrine)8, and an existing drug with a novel delivery system9. Research is also being done to improve the diagnostics of this disease and to enable earlier detection of airway inflammation10. COPD is currently an irreversible disease, and there are attempts to find new molecules that will help cure or reverse the disease. However, these are still in the investigative stage and a long way from becoming part of the standard of care.
Clinical Trials
Clinical trials are how pharmaceutical companies test their new drugs. The drugs are usually on their later stages of development and are aimed to potentially cure COPD or improve the medications, treatments, and therapies that are already on the market. By participating in clinical trials, patients are given the chance to try a potential cure and to play a large role in the advancement of COPD research. After all, most of the current treatments are available and accessible because of their success in previous clinical trials!
The hardest part about these studies is finding enough patients to participate, so researchers are constantly looking for more participants! Both patients and researchers gain from these clinical trials. All patients have to do is meet the eligibility requirements for the different trials, like age, gender, stage of disease, and previous treatments. The benefits of clinical trials include the following:
- Participants are given advanced treatment and therapy that isn’t even available to other patients
- Participants usually receive better health care than others
- Participants have the chance to play an important role in finding treatments that could later help COPD patients all over the world
- Participants are sometimes paid for participating in studies
- Participants are monitored closely during and after the study to ensure their safety
Some current clinical trials are already on their way to making life changing discoveries. Some of these studies include the following:
PREVENTION OF ACUTE WORSENING OF COPD
The goal of this study is to test a new drug called metoprolol on patients and to measure its effect on exacerbations. It will be studied by measuring the time until the patient acquires the first exacerbation after using the drug, and the severity of such exacerbation.
SPIRATION VALVE FOR EMPHYSEMA TO IMPROVE LUNG FUNCTION
The goal of this study is to improve the lung function for people living with emphysema by testing a new treatment called the Spiration Valve. The spiration valve is a small device placed in the airways of the lungs for the purpose of redirecting airflow to healthier parts of the lungs.
New Clinical Trials
There are many more studies available to patients to participate in and benefit from all over the world. New and more advanced research on COPD is also being discovered every day because of these studies. The following are some of the newest clinical trials that are available to qualified patients.
Match to COPD Clinical Trials
Conclusion
Chronic obstructive pulmonary disease (COPD) can seem to make living a normal life difficult at times; however, with the right treatments and attitude, living with COPD is not impossible. In fact, many patients are surprised at what they can accomplish after receiving the right treatments and making healthy changes in their lifestyle! Furthermore, clinical trials and research are actively studying even better therapies and potential cures. The more patients participate in these studies, the faster these potential therapies and cures can become available to and help all COPD patients!
References
- Global Initiative for Chronic Obstructive Lung Disease. Accessed July 27, 2020. https://goldcopd.org/
- DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L. eds. Pharmacotherapy: A Pathophysiologic Approach, 10e. McGraw-Hill; Accessed February 23, 2021. https://accesspharmacy.mhmedical.com/content.aspx?bookid=1861§ionid=146028752
- Anoro Ellipta. Package Insert. GlaxoSmithKline; 2013. https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/203975s000lbl.pdf
- Stiolto Respimat. Package Insert. Boehringer Ingelheim; 2016. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/206756s006lbl.pdf
- Trelegy Ellipta. Package Insert. GlaxoSmithKline; 2017.
- https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/209482s000lbl.pdf
- Package Insert. Forest Pharmaceuticals; 2013.
- Labarca G, Uribe JP, Pacheco C, et al. Bronchoscopic Lung Volume Reduction with Endobronchial Zephyr Valves for Severe Emphysema: A Systematic Review and Meta-Analysis. Respiration. 2019;98(3):268-278. doi:10.1159/000499508
- Dose ranging study of RPL554 in COPD patients. https://clinicaltrials.gov/ct2/show/study/NCT03443414?term=RPL554&recrs=e&rslt=With&draw=2&rank=4
- Donohue JF, Goodin T, Tosiello R, Wheeler A. Dose selection for glycopyrrolate/eFlow(®) phase III clinical studies: results from GOLDEN (Glycopyrrolate for Obstructive Lung Disease via Electronic Nebulizer) phase II dose-finding studies. Respir Res. 2017 Dec 4;18(1):202. doi: 10.1186/s12931-017-0681-z.
- Vasilescu DM, Martinez FJ, Marchetti N, et al. Noninvasive Imaging Biomarker Identifies Small Airway Damage in Severe Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2019;200(5):575-581. doi:10.1164/rccm.201811-2083OC