Match to Osteoarthritis Clinical Trials
What is Osteoarthritis?
Osteoarthritis, also known as OA, is a degenerative joint disease and the most common type of arthritis. It affects the cartilage in the joints and the underlying bone tissue. It usually affects hips, knees, neck, back, and the small joints in fingers and toes; however, it can occur in any other joint in the body.
Its symptoms include joint pain which worsens with exercise and improves with rest, loss of movement, joint stiffness after rest, joint swelling or deformity, crackling of the joints (called “crepitus”), along with the absence of systemic symptoms, such as fever, which means that the disease isn’t infectious and only affects the musculoskeletal system.Hard bony masses, called Heberden’s or Bouchard’s nodes depending on their location, can appear in smaller joints. In some cases, osteoarthritis can be asymptomatic.
What Causes Osteoarthritis?
Osteoarthritis occurs when the body can’t repair the normal wear-and-tear on the joints. This can happen because the repair process becomes faulty, or because of excessive wear on the joints. Bones can also be misaligned due to congenital conditions, excessive weight, and injuries.
When joints are affected by osteoarthritis, there is excessive cartilage degradation; substances released from the breakdown of cartilage can also induce a mild inflammatory response which affects the joint and its surrounding structures.
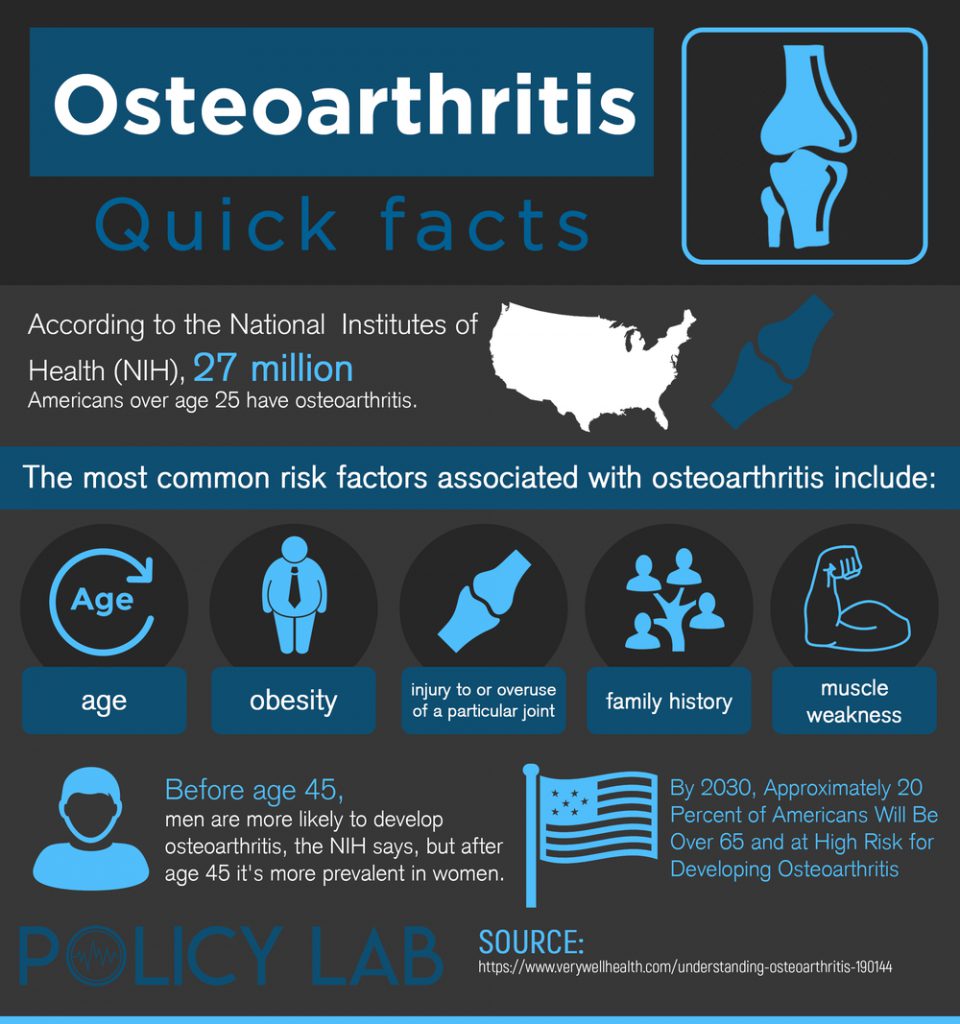
There are several risk factors which can increase the risk of osteoarthritis. Some of these factors include:
- Age
Osteoarthritis becomes more common as age advances. - Obesity
Joints suffer more strain if they are exposed to excessive body weight. This is especially true for hip and knee joints. - Gender
The condition is more common in postmenopausal women than men of similar age. This could be due to changes in hormonal levels. - Genetics
Studies have shown that osteoarthritis is more prevalent in siblings, which points to a hereditary component. - Work or Hobbies
Certain professional fields have greater exposure to joint wear than others. For example; elite athletes, workers who used pneumatic drills, working in constant squatting or standing positions, climbing, etc. - Previous Joint Injury
Previous injuries, fractures, or infections can predispose the joint to suffer greater cartilage degradation.
Match to Osteoarthritis Clinical Trials
How is Osteoarthritis Diagnosed?
Osteoarthritis can usually be diagnosed with some certainty based on a patient’s age, medical history, symptoms, and physical examination. Doctors may order x-rays to confirm the diagnosis; these will show several changes, such as narrowing of the joint spaces. These changes will confirm the osteoarthritis diagnosis.
There are also standardized criteria which are used to diagnose hand osteoarthritis based on clinical symptoms. Other tests, such as blood tests or an MRI may be ordered to rule out other causes of joint pain. There are also several classification systems used to categorize the disease, depending on the affected joints, its severity, and whether it is primary or secondary to an underlying cause.
Treating Osteoarthritis
Although osteoarthritis can’t be cured, several medications are used to manage the symptoms it produces, thus improving the patient’s quality of life. Some of these medications include:
- Acetaminophen or paracetamol: this is the most commonly used painkiller for osteoarthritis, and it works for mild to moderate cases.
- Non-steroidal anti-inflammatory drugs (NSAIDs): such as naproxen or diclofenac. These are also used for mild to moderate cases, but they have a higher rate of side effects, such as gastrointestinal symptoms. They can also be taken during short periods of time when symptoms flare up, returning to acetaminophen when they improve. NSAIDs can also be used topically.
- Opioids: such as tramadol, are usually only prescribed when acetaminophen and NSAIDs have failed.
- Glucocorticoids: these can be injected into the affected joints, and provide short-term improvement. They include hydrocortisone, and recent research has suggested triamcinolone could also be effective.
- Duloxetine: although this medication is more commonly used as an antidepressant, it has been shown to improve osteoarthritis symptoms such as pain and functional impairment.
- Herbal creams: although they aren’t meant to be used as the primary therapeutic option, some herbal creams and gels can increase symptom relief. They include arnica, capsaicin, and comfrey.
- Mesenchymal stem cell therapy: this method is currently being research, but studies have shown it is a promising option for knee osteoarthritis.
Osteoarthritis Clinical Trials
Osteoarthritis is the most common type of arthritis and a very important cause of disability; therefore, clinical trials are often carried out to discover a way to cure it, and to test out new treatments meant to improve the quality of life of those who suffer from it. Clinical trials are also performed to find more effective ways to prevent and diagnose this illness.
Clinical trials are led by a team of medical specialists and researchers, and carried out in universities, hospitals, and research centers. They allow the participants to exert more control in how they choose to manage their illness; however, it is important to note that any patient can withdraw from clinical trial at any point if they wish to do so.
If you suffer from osteoarthritis and are interested in joining a clinical trial, contact your doctor, or research organizations to receive more information on clinical trials available to you and how to enter them.
Lifestyle Changes
Lifestyle changes are usually recommended to osteoarthritis patients, since they can help manage their symptoms and improve their quality of life. Some of these changes include:
- Weight loss: losing excessive weight will lessen the load that joints have to support, which can help reduce cartilage degradation and improve symptoms.
- Exercise: working out at least three times a week has been shown to improve pain and movement. Exercise should be approved by a doctor or physical therapist to reduce the risk of injuries.
- Heat and cold therapy: applying cold or hot packs, or towels can reduce stiffness and pain.
Tips for Friends and Family
- Be understanding if your loved one can’t accompany you to certain activities or keep up the pace. Come up with things you can do together that won’t be painful for them.
- Let them know you are there if they need to discuss or vent about their diagnosis.
- Offer help when they are faced with challenging tasks.
- Make sure your home is a safe environment for them, by improving lightning or removing objects which could injure them.
- Help them stick to their lifestyle changes and self-care strategies, such as eating a balanced diet, exercising regularly, and applying heat and cold therapy.
Match to Osteoarthritis Clinical Trials
Sources
- Osteoarthritis. Medicine Net. Recovered from https://www.medicinenet.com/script/main/art.asp?articlekey=90187
- Imm, N. Osteoarthritis. (March 7th, 2017). Recovered from https://patient.info/health/arthritis/osteoarthritis