Match to Hepatitis C Clinical Trials
What is Hepatitis C?
Generally speaking, hepatitis is a disease caused by an inflammation of the liver. This can be caused by a number of things, such as alcohol, toxins, autoimmune disease, and more commonly, viruses.
There are five types of viral hepatitis, called hepatitis A, B, C, D, and E. Each type is caused by a different virus and has different characteristics, but they all affect the liver.
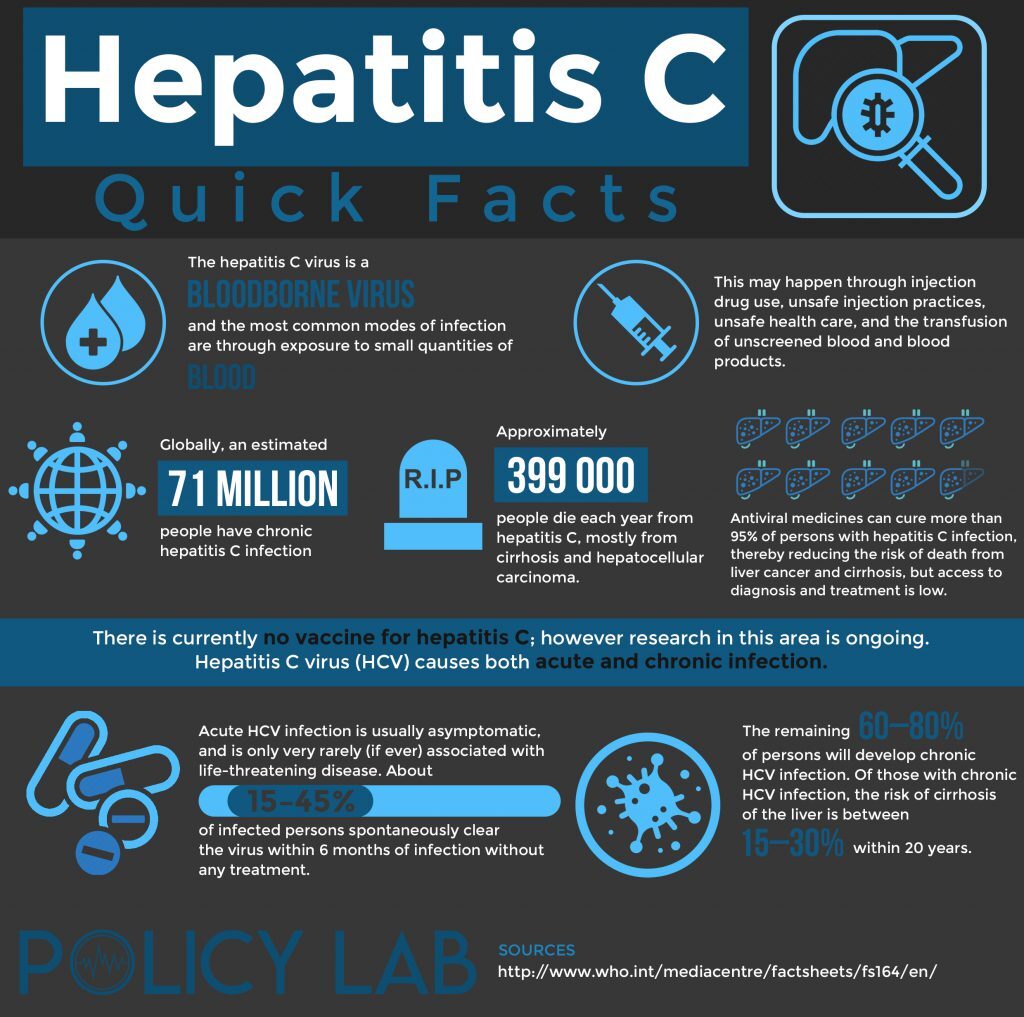
The World Health Organization estimates that approximately 3% of the world’s population has been infected with Hepatitis C, making it one of the most prevalent blood-borne diseases in the world. There are a number of treatment options for Hep C, and ongoing clinical trials and research are searching for a cure.
What Causes Hepatitis C?
Hepatitis C is caused by the Hepatitis C virus, sometimes shortened as HCV. Even though some patients will develop acute symptoms shortly after being infected, most patients can remain symptom-free for years or even decades, developing a chronic condition which is only diagnosed later in life when symptoms start to appear. In addition to damaging the liver, HCV can also affect the digestive, nervous, and immune system.
Hepatitis C is transmitted when blood that carries HCV enters the circulation of a healthy person. This can happen through the use of contaminated needles, which usually happens as the result of sharing needles for drug use; infection through sharing personal items, unprotected sex, tattoos or piercings, work accidents, and donated blood are also possible, but less common.
There are six types of Hepatitis C virus, all of which have different genes. They’re labeled as genotypes and numbered from 1 to 6. It is also possible to suffer from an infection caused by more than one of these genotypes at the same time.
Match to Hepatitis C Clinical Trials
How is Hepatitis C Diagnosed?
Diagnosing Hepatitis C depends on when the symptoms occur, since this usually determines the moment when the person affected seeks medical help and is diagnosed with the disease.
It is estimated that only 20% to 30% of patients develop acute symptoms, which occur within 1-6 months after being infected with the virus. These symptoms include lack of appetite, fever, fatigue, jaundice (yellow discoloration of the skin and eyes), nausea, vomiting, dark urine, and abdominal pain. Extrahepatic symptoms can also occur, such as arthralgias (joint pain), paresthesias (sensitivity disorders), myalgias (muscle pain), and pruritus (itchy skin).
More commonly, though, patients don’t develop any acute symptoms and instead progress to a chronic infection, which only causes symptoms after serious liver damage occurs. This can happen decades after the initial infection. Amongst the symptoms that can develop with chronic liver damage, patients can suffer from inexplicable weight loss, pruritus, coagulation disorders that cause the patient to bleed and bruise easily, chronic fatigue, jaundice, ascites (abdominal fluid buildup), swollen legs, spider angiomas (spider-like blood vessels on the skin), hepatic encephalopathy (slurred speech, confusion), vomiting blood (hematemesis or melena caused by variceal bleeding), gynecomastia.
Once the patient seeks medical assistance and Hepatitis C is suspected, an anti-HCV tests is used to detect the presence of antibodies to the virus; however, this test doesn’t differentiate between an active or previous infection. To confirm a result, a HCV RIBA test is ordered to confirm whether the infection is active. Tests are also carried out to determine the HCV genotype. A liver biopsy may be carried out if the diagnosis is unclear, but it isn’t mandatory.
After a Hepatitis C diagnosis is confirmed, the patient should also be tested for HIV and Hepatitis B, since these diseases are transmitted the same way as HCV.
Treating Hepatitis C – Cures & Medicines
While there isn’t –currently- a vaccine to prevent Hepatitis C infection, patients are encouraged to get vaccinated against Hepatitis A and B.
The traditional regime to treat Hepatitis C includes pegylated interferon –also known as peginterferon- (Pegasys) and ribavirin (Copegus). Treatment is usually started somewhere between 2 to 4 months after the onset of the disease, since there is a possibility of spontaneous viral clearance within 6 months of the infection.
Patients with advanced hepatic fibrosis, cirrhosis, severe extrahepatic symptoms, high-risk for complications and transmission of the disease are given priority for treatment. Treatment of Hepatitis C aims to eradicate the virus and to prevent the progression to cirrhosis or hepatocellular carcinoma.
Newer medications include direct-acting antivirals (DAAs) and polymerase inhibitors, such as simeprivir, ledipasvir, elbasvir, grazoprevir, and sofosbuvir. These medications have been approved for use after being tested in clinical trials, and can be given in combination with peginterferon and ribavirin, or by themselves.
In severe cases of Hepatitis C, a liver transplant may be necessary.
Interview with an Expert

Dr. Lijo John
Dr. Lijo John is a community pharmacist with 9 years of experience and graduated from Rutgers University in 2012. He has extensive experience serving patients with a focus in geriatric medicine, diabetes management, and preventative medicine such as immunizations and lifestyle modification counselling. Dr. John also enjoys writing and presenting on complex medical topics aimed at the general population to drive positive behavioral change in topics such as vaccine hesitancy and smoking cessation.
An Overview of Hepatitis C
Hepatitis C (HCV) is an insidious and chronic infection that affects approximately 3.2 million people in the United States. HCV is prevalent in high-risk populations such as injectable drug users, the homeless and prisoners. Most acute HCV infections are asymptomatic, which means there is usually significant disease progression before it is diagnosed.
How Has Treatment Developed Over Time?
Almost all patients with HCV infection are recommended for treatment, and the treatment goal is to cure the disease. Sustained virological response (SVR) is defined as no detectable viral load 12 weeks or later post completion of therapy. The current treatment for HCV for is an oral drug regimen of Direct Acting Anti-virals (DAA’s) lasting 8 to 12 weeks.
What is the Current Standard of Care?
The standard of care for HCV infection in the 1990’s was Interferon (IFN) alpha-2b. The SVR rate for this therapy was only 15%, which was enhanced to 41% following the addition of ribavirin (RBV) after 48 weeks of treatment. Pegylated IFN + RBV incrementally improved the SVR to approximately 50%, but this was still affected by various factors such as length of therapy, and the strain of HCV being treated. This therapy also had a significant side effect profile such as flu-like symptoms, neuropsychiatric symptoms like depression and irritability, as well as possible autoimmune exacerbations.
What Are Some Newer Treatments?
The approval of DAA’s starting in 2013 ushered in a new era in HCV therapy with SVR approaching 100% with just 8 to 12 weeks of therapy and relatively minimal side effects. HCV has several strains and more may yet be identified. Treatment decisions depend on the strain of the virus, patient’s past treatment history and whether cirrhosis is present. Advances in therapy will most likely come from improvements in sequencing the virus and allowing for optimal therapeutic choice. Next generation sequencing (NGS) is crucial to this next leap as this will provide a rapid and effective method of genotyping the virus and identifying resistant variants. There are also on-going trials investigating new DAA’s, but with cure rates already approaching 100%, it remains to be seen how much marginal benefit there will be from additional approvals. The main challenge that remains is improving access to patients that need to be screened, diagnosed and treated.
Hepatitis C Clinical Trials
Hepatitis C trials are frequently conducted, given the disease’s high prevalence and risk for life-threatening complications, which makes preventing and curing the disease a top priority for investigators and healthcare workers.
The new drugs which have been approved for treatment of HCV have all gone through extensive medical trials to determine their efficacy, security, and to ascertain which genotypes they work best against. There is also great interest in developing a vaccine which can prevent infection, or its progression to chronic Hepatitis C.
If you are interested in joining a clinical trial for Hepatitis C, you can search online for open trials in your area, ask your doctor about clinical trials, or contact hospitals or universities and request information. In order to participate in a clinical trial, you need to meet certain criteria which is determined by the research team to ensure maximum accuracy in the trial’s results. Also, it is important to remember that you can always leave a clinical trial if you desire to do so.
Lifestyle Changes
If you are living with Hepatitis C, certain lifestyle changes can help lessen its symptoms and progression, and improve your quality of life.
- Avoid alcohol ingestion.
- Get vaccinated for Hepatitis A and B.
- Avoid medications that can cause liver damage.
- Help prevent the disease by making sure other people don’t come into contact with your blood.
- Don’t use illicit drugs.
- Practice safe sex.
- Maintain a healthy weight and diet.
- Drink at least 8 glasses of water each day.
- Visit a therapists if you are feeling fear or anxiety over your diagnosis.
Tips for Friends and Family
- Make sure your loved ones understand what Hepatitis C is, and how it is transmitted.
- Talk to your family, sexual partners, spouse, and anyone else who may have caught the disease from you so they can get tested.
- Ask your loved ones for emotional support while you go through diagnosis and treatment.
- Educate your family members on how to properly clean up blood, in case any injuries occur.
- Keep your own personal hygiene items and jewelry, such as earrings, separate from those of your family members.
- Additional information on autoimmune hepatitis clinical trials is included here
Match to Hepatitis C Clinical Trials
Sources
- Things You Should Know About Hepatitis C. 2012. Retrieved from https://www.acponline.org/journals/annals/intheclinic/itc-hepatitis-c-2012-patient-information.pdf
References
- DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L. eds. Pharmacotherapy: A Pathophysiologic Approach, 10e. McGraw-Hill; Accessed February 23, 2021. https://accesspharmacy.mhmedical.com/content.aspx?bookid=1861§ionid=146028752
- Fung J. Era of direct acting antivirals in chronic hepatitis C: Who will benefit?. World J Hepatol. 2015;7(24):2543-2550. doi:10.4254/wjh.v7.i24.2543
- Dusheiko G. Side effects of alpha interferon in chronic hepatitis C. Hepatology. 1997;26(3 Suppl 1):112S-121S. doi:10.1002/hep.510260720
- Sanaa M. Kamal (March 8th 2017). Advances in Treatment of Hepatitis C, Advances in Treatment of Hepatitis C and B, Naglaa Allam, IntechOpen, DOI: 10.5772/66719. Available from: https://www.intechopen.com/books/advances-in-treatment-of-hepatitis-c-and-b/advances-in-treatment-of-hepatitis-c#B114